By Dr. Dale Macdonald
@EliteSportYYC
Elite Sport Performance / The Knee Clinic
Calgary, AB CANADA
In this article, I am going to be boiling down many of the different potential injury mechanisms that pertain to distance running. Drawing both from what the literature and my own professional experience suggest may be the seven most causative factors contributing to running injury. The first amongst these, and in no particular order, are:
Error #1: Excessive Impact forces.
Impact forces exist and occur when we first strike the ground during a stride. When we walk, impact forces of approximately 1.5 times our body weight are absorbed over approximately 50 milliseconds, while impact forces with running can range between 4 and 8 times our body weight, and accrue over only 10 to 30 milliseconds. The difference here is that we are absorbing a significantly higher amount of impact in a significantly shorter amount of time while running, as opposed to walking. Determinants of impact forces include:
- the foot velocity at contact,
- the effective mass of the body at contact,
- the contact area of the foot and the actual foot shape during impact
- the angle of surface, i.e. downhill versus flat ground
- the material properties of such things as:
- connective tissues,
- the cushioning properties of our shoes,
- the surface we choose to run on
- any insole or orthotic that we are choosing to wear.
As alluded to in point #3 above, the shape of our foot will greatly influence how that force is transmitted up the rest of the lower limb.
The term for the natural collapse of the mid-foot during the mid-stance phase of gait is pronation. Pronation is a protective mechanism that exists naturally during gait, including both walking and running. Pronation allows impact forces to be spread over a longer period of time during the stance phase of gait.
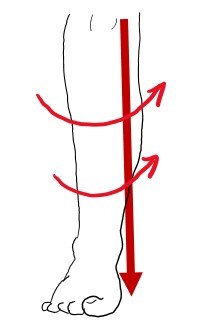
Pronation has a bad reputation but inherently is inappropriate; it is only a problem when the amount of pronation falls outside of the normal physiological limits or if it continues too long beyond mid-stance. Pronation starts an entire internal rotation biomechanical chain of events from the ankle through the shin into the medial part of the knee, up through the IT band, and ultimately into the hip, pelvis and lumbar spine.
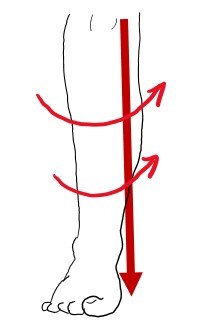
The degree of this internal rotation influences how certain structures in the lower limb are subjected to these impact forces. Impact forces are also influenced by whether or not we are rear-foot strikers, mid-foot strikers or forefoot strikers.
Over 80% of all runners are naturally rear-foot strikers. While this is inherently quite fine, rearfoot strikers are repeatedly subjected to abrupt, decelerating, collision forces within the first 50 milliseconds of ground contact. Interestingly, however, peak impact is not during initial heel strike; rather, peak impact happens about 30 milliseconds after initial heel strike when we are truly in the mid-stance phase of gait at the very time when pronation is most important.
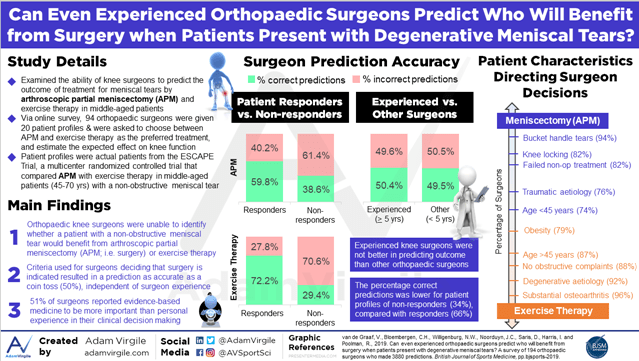
People in today’s society are often caught up in current trends with respect to footwear and how that footwear may mitigate or dissipate impact force in general, but a more appropriate question may be ‘how does a shoe dissipate peak impact forces?’. The graph below illustrates the difference between initial heel strike and peak impact force absorption

Error #2: Poor Footwear
Contemporary shoes, that is to say, normal typical neutral shoes, are not as good as they need to be. Despite the incredible advances in running shoe technology, injury rates have not declined in 30 years. The problem with contemporary shoes stems at least in part from their limited ability to deal with anatomical realities. We have 37 different bones within the foot and ankle, all working to manage these maximal impact loads. There is very little conversion of energy in these structures below the ankle; most of it is lost to collision. What is not lost to collision is absorbed into various tissues as potential / elastic energy, able to be recoiled back as kinetic energy to help propel us forward. The collision force ends up creating injurious shock waves, which we will talk about later in point #6.
There are several ways to tell if your shoes are appropriate or not and I discussed this in a previous article titled, “Five Ways to Tell if Your Shoes are Worn Out”.
In recent years, more and more people have turned to barefoot running as a way to avoid or modify how much impact force they absorb. For the purposes of this next section, barefoot running is defined as running truly barefoot….no shoe or covering of any kind. With true barefoot running, impact peak occurs towards the front of the foot. The ankle dorsiflexes as the heel drops under control of the arch, calf, and Achilles. Forefoot strike happens in front of the hinge of the ankle, which helps to rotate the leg forward.
Barefoot running allows you to soak up the impact better than shod running with not only the feet but also the ankles, knees, and even the hips. Furthermore, bare feet are more sensitive to different running surfaces. You will run softer on hard surfaces due to the proprioceptive input of having the skin actually touching the ground. Furthermore, barefoot running reduces energy expenditure by approximately 5% as compared to shod running at the same speed. Peak vertical force absorption at impact is about one-third as much, i.e. 66% less, than heel striking when wearing regular shoes. To make sense of this, imagine tip-toeing as you try to walk very quietly; your hips, knees and ankles all have to bend more in order for you to walk quietly. In this same fashion, barefoot runners absorb force more gradually than shod runners do, and they absorb it over a longer period of time.
Barefoot running allows for better use of the plantar fascia and Achilles as natural elastic sources of recoil. Some additional advantages of running barefoot include reduction in overall injury rates, increased muscular strength, decreased cost and decreased risk of foot deformities. Barefoot running offers also the opportunity for significant alterations in runner’s gait, reduction of impact forces, improved running economy, and improved proprioceptive feedback.
It is not, however, without its own deficits. Some of the disadvantages of barefoot running include injury from actual running surface debris and general hazards, thermal injuries from running surface extremes of temperature, the availability of adequate surfaces on which to run, and exposure to infectious agents or microorganisms. Barefoot running is bad for runners who require control for existing conditions because it allows for loss of protective sensation, it magnifies the shockwaves created initially at impact and increases shock transmission to back muscles.
Orthotics are another way to mitigate impact. Custom orthotics are most effective at reducing exercise-related leg pain. They work in 75-88% of cases of distance runners suffering leg pain. There are large benefits for those with plantar fasciitis and moderate benefits for the prevention of tibial stress fracture and patellofemoral pain. The material composition of orthotics matters. A foam-top cover helps to adapt to foot shape while a firm shell provides a more direct feedback from the running surface and enhances proprioceptive input. Contrary to popular myth, orthotics do not contribute to atrophy of the muscles of the feet. Rather, they heighten the stimulation of intrinsic proprioceptors within the foot, stimulating better neuromuscular control.
Error #3: Poor form (inadequate strength).
Fascinatingly, there is no difference in total energy cost between good runners and bad runners. Good runners simply waste less energy. What this is means is that good runners can run faster at the same degree of energy cost that bad runners can, running more slowly.
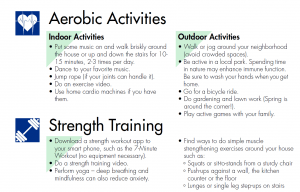
Poor form leads to adaptation of fascia and connective tissue. In fact, good form also leads to these same adaptations. In order to create adaptation of fascia and connective tissue to exercise, we need to train hard enough to get a tissue response. This looks something along the lines of eight repetitions of weightlifting at 70% of our one repetition max within 30 seconds in order to produce a significant protein release for muscle growth.
Training increases the number of connections between tendon and muscle and a tendon/muscle interface strengthens by wrinkling tighter and tighter together over time. Individual muscle fibers go from one end of the muscle all the way through to the other end. Once a muscle fiber is damaged, damaged fibers do not just try to reattach, rather they have to grow all the way back to their other attachment point. This takes significant time.
Error #4: Ignoring pain.
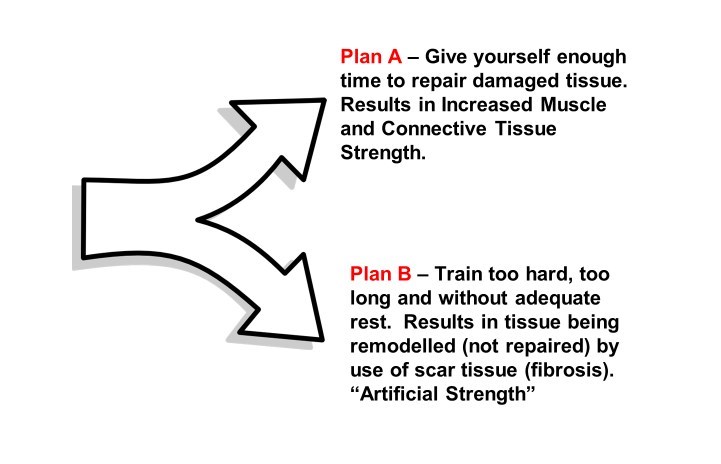
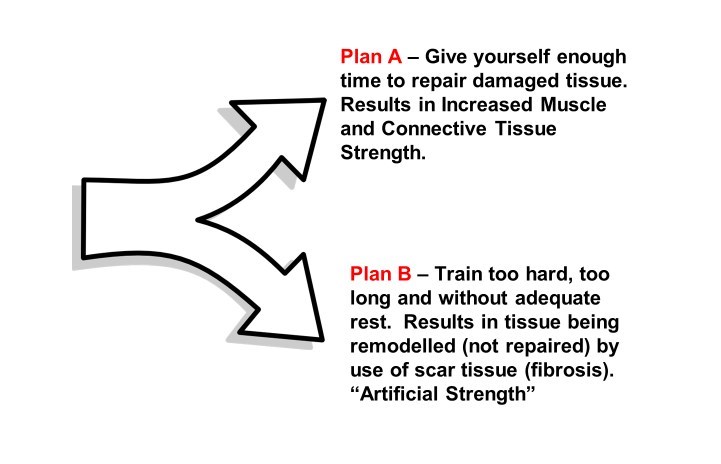
This deadly sin is one of the most common. Our body is constantly trying to convey information to us, but it is up to us to be able to pay attention, listen to the signals and interpret them correctly. Running is a highly competitive activity and running injuries are common. All overuse running injuries are the result of training errors. Our body has two options – Plan A or Plan B. Plan A is tissue repair. This happens when we give ourselves enough time to repair damaged tissue between bouts of exercise. Tissue report results in increased muscle and connective tissue strength. If we train too hard, too long, or without enough rest, we start to enact Plan B.
Plan B is tissue remodeling. With tissue remodeling, the tissue is not repaired but instead remodeled through the deposition of scar tissue/fibrosis. This allows the area to become artificially tight but not capable of doing its job in an elastically correct manner. Ignoring pain leads to repetitive strain injuries and these injuries show up out of the blue but they are not sudden. We can be out for a long Sunday run and all of the sudden, begin to start feeling pain in an area that has been previously asymptomatic. In reality, this is not a new injury but rather the culmination of training too hard, too long, or without enough rest for an extended period of time. Remember that absence of evidence is not evidence of absence.
Just because something does not hurt does not mean that you are biomechanically training perfectly. You ignore pain signals at your peril. One of the guidelines that I give to patients is to differentiate hurt versus harm. It is okay for something to hurt while we run so long as it is not causing sharp pain or causing us to limp or change our gait. If either of those two things happen, you are very likely going to be causing more harm.
Error #5: Excessive duration.
In a world where Ironmans, ultra-marathons and death races are popular, it is easy to think that these incredible athletes are doing things right and with no detriment to them. Nothing could be further from the truth, however. The degree of muscle damage that a runner incurs is directly proportional to the distance run. There is no adaptation to the distance at a cellular level; muscle breaks down at the same rate regardless of how fit we are. Interestingly, and for reasons not fully understood, men have higher markers of muscle damage than women do for a matched distance. We begin to see increased calcium accumulation in muscle after approximately 20 kilometers of running due to muscular cell wall damage. Muscle damage continues and the body begins to display symptoms of exercise induced muscle damage. These symptoms include, but are not limited to:
- delayed onset muscle soreness,
- increases in volume and circumference of the limb,
- decreases in range of motion,
- decreases in muscular strength,
- leakage of intracellular proteins into the blood, and
- muscle fiber swelling.
Muscle fatigue begins within 14 minutes of running. This causes a loss of consistency in form and a decrease in muscle stiffness. This decreased stiffness sounds paradoxical but creates a loss of muscle’s elasticity and ability to act as an uncomplicated spring.
Other sequelae of distance running exist as well. The literature shows a reduction in spinal cord activation levels of 8% after three hours of running. Running for periods between two and eight hours reduces our maximal knee extensor voluntary contraction by between 19% and 35%. This has significant consequences on our running technique and consequently increases our risk of injury. It’s important to note that this reduction in strength is not all from local, muscular damage. There are several sites for strength loss due to fatigue:
- Our cerebral cortex begins to send poorer quality signals.
- Our spinal cord begins to send impaired signals.
- The neuromuscular junction begins to be impaired.
- Even contractile fibers in the muscle become impaired and we finally get inhibition from sensory fibers that are yelling at the rest of our body, trying to get us to stop running.
With the onset of fatigue, we get an increase in the overall cost of running and an increase in stride variability, both of which are associated with increased risk of injury. Our total energy cost of running increases as we fatigue, and we become far less efficient as a consequence.
Ultramarathons (50km or more) in particular, trigger a temporary inflammatory response of a similar nature to trauma, burn, surgery or even sepsis. Researchers have demonstrated liver damage markers equivalent to severe liver injury by way of blunt motor vehicle trauma. Studies have even measured heart damage markers similar to levels seen during an acute heart attack. These markers have been recorded in certain Boston Marathon records at up to 500% higher than normal heart damage markers.
Our heart begins to work less well as we continue to run longer and longer distances. The 2006 Boston Marathon study showed that 60% of those tested showed markers of heart cell damage. A 2008 study found the incidence to be 86% of runners. The average runner can lose 10 pounds of sweat during a marathon, during which time 40,000 heartbeats occur. The loss of such high volumes of fluid as sweat significantly changes the volume of blood that our heart pumps, altering both the stroke volume (heart chamber filling) and blood pressure. This reduction in stroke volume continues for a period of time even after the run. There are more than 21 studies to date showing these significant heart health impairments due to long distance running.
Lastly, we see red blood cell damage. This is present in all athletes and it is due to many factors, including muscle contraction, crushing the actual red blood cells. This red blood cell damage increases up to a point, i.e. around the three-hour mark, then stays constant independent of the speed or further distance.
Error #6: Inadequate work hardening.
Wolff’s law states that the remodeling of tissue is influenced and modulated by mechanical stresses. Repetitive strains lead to tissue overload. As one tissue fails in a particular chain, the next tissue will then absorb even greater force and be more readily brought to the point of failure itself. A good example of this is with respect to medial tibial stress syndrome, AKA shin splints. Ten to twenty percent of all runners will get shin splints at some point in their running career. Not coincidentally, regional bone density is 12% lower than normal when you are symptomatic for shin splints, and bone mineral density increases by 19% once the pain goes away as bone forming cells (osteoblasts) ramp up their activity level. Recall that it is the rate of loading, not the peak impact force, that causes medial tibial stress syndrome.
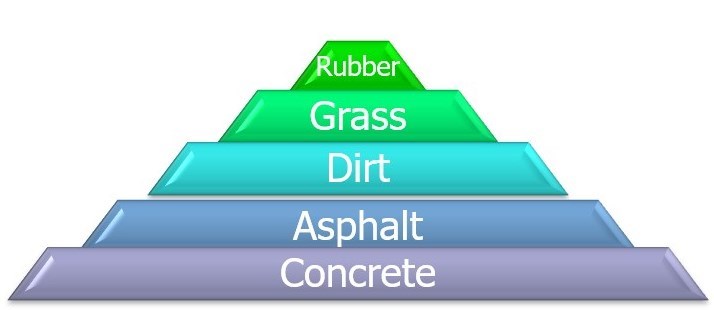
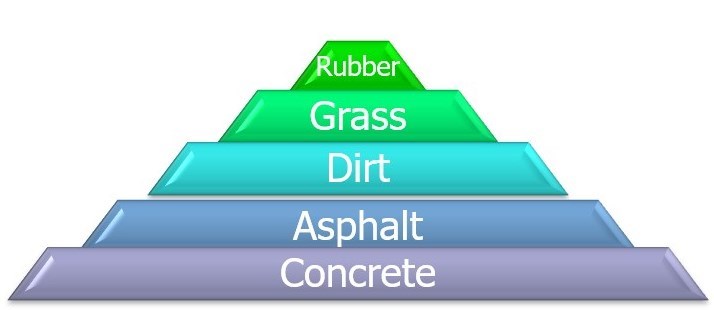
Various running surfaces, as mentioned before, can influence how much force and shock we absorb. Running on a rubberized track is best followed by grass or a cushioned treadmill. Dirt, asphalt and then concrete are in order progressively harder and harder surfaces. Running on a modern rubberized track results in a 12% decrease to a runner’s metabolic rate and allows a 29% increase in their leg stiffness. Increased leg stiffness is advantageous in a distance runner as it actually improves kinetic return of energy and increased efficiency. Proper track materials can improve performance by 2-3% and can decrease our rates of injury by up to 50%. A rubberized track will promote a greater spring in the legs, allowing you to more naturally drive the knees up.
Error #7: Inadequate rest.
There are three kinds of recovery that are pertinent to runners.
- The first is immediate recovery, the micro-time between each gait cycle.
- Short-term recovery happens between repeats that we do during training, the walking back section between intervals.
- Training recovery is that which occurs between individual workouts.
There are significant immune system implications related to the amount of rest that we get. Intense and/or prolonged exercise creates oxidative stress and immune suppression for a period of time. If this is done repeatedly without adequate rest, there can be an additive immune depleting effect.
This brings to mind the question, should you run when you are sick? Having a cold with no fever and energy levels that are only mild depressed, it is relatively safe to exercise at up to about 60% intensity (roughly 60% of our VO2 max). In other words, it is okay to go for an easy run no longer than one hour.
You should skip your run if you have the following symptoms:
- Fever,
- moderate-to-severe energy depletion,
- systemic symptoms such as muscle aches or pains that are not related to training,
- diarrhea, vomiting, or a high resting heart rate relative to normal.
Training too much can lead to patchy myocardial fibrosis or scar tissue within the heart wall. Scar tissue of this nature can, just like in any other muscle, create significant problems. In the case of the heart, arrhythmias, coronary artery calcification, and arterial wall stiffness are also known effects of training too much.
Error #8: Poor nutrition.
Just as you would not put a very poor-quality fuel in your vehicle, so too should we be conscientious about how we fuel our bodies. Eating carbohydrates before prolonged exercise is proven to help reinforce our immune system. Eating a combination of proteins and carbohydrates immediately after strenuous exercise, as well as during prolonged exercise, helps to moderate the negative effect distance running can have on immune function.
Many runners experiment with carbohydrate loading but there is a best-evidence based way to do this. Interestingly, the rate of carbohydrate repletion during carbo-loading is enhanced by the degree of depletion immediately before. Said another way, we fill up faster if we have emptied our tank first. Timing is everything however; the sooner we can ingest these carbohydrates after an intense workout, the better repletion rates we achieve.
During periods of carbo-loading, an adequate daily carbohydrate intake is between 7 and 10 g/kg of body weight. For correct carbohydrate loading, at one-week pre-race, you should exercise very little to not at all and eat normally. Between 24 and 36 hours before the race, there needs to be one vigorous exercise bout of 20-30 minutes duration in order to bottom out your carbohydrate load. This can be something along the lines of a 5-kilometer speed / tempo run for a marathoner. One to three hours after that workout is when your glycogen window is wide open for optimal carbo-loading at the 7-10 g/kg formula mentioned above.
Many people try to consume some carbohydrate during their running, but often this causes stomach issues. Recent research has shown promise for something called carbohydrate mouth rinsing. Mouth rinsing, that is to say sloshing around and then spitting out a 6% carbohydrate solution, increases self-selected speed, reduces significantly gastrointestinal irritation and increases the distance that a person can run over a 1-hour period. Furthermore, it enhances the feeling of pleasure, giving us that runner’s high, and it’s mechanism of action is postulated to be linked to fueling the brain directly through the hard and soft palate at the roof of your mouth.
Proper hydration is obviously important. As a general guideline, 2-3 cups of water should be ingested 60-90 minutes before a run. Once you are running, consume 1 cup of a sport drink every 15 minutes; this is roughly equivalent to 60 g of carbohydrate per hour. After a run, it is recommended to ingest 140-160 g of carbohydrate within 2 hours. This is not needed should your run be less than 90 minutes long. Remember, “a great diet cannot make an average athlete elite, but an average diet can make an elite athlete average”.
Without doubt, there are many other errors that distance runners can, and do, make, but the aforementioned eight are the most common methods used by runners to end up in an office like mine. Running is one of the healthiest things that we can do for ourselves, improving our health, our state of mind and measurably extending our morbidity free years. Listen to your body, pay attention to the details and work to conscientiously avoid the eight errors outlined above and you too can enjoy all the good that running has to offer.